An inevitability of living with persistent pain is that you experience ‘flares’ from time to time.
My simple understanding of a pain ‘flare’ is that they are times when you experience significantly increased pain for an extended period of time.
This blog on pain ‘flares’ was written at the same time as a blog on ‘pacing’ and ‘wind up pain’. In order to fully understand this blog then it would be helpful to read my blog on ‘pacing’ and ‘wind up pain’ first. It can be found HERE.
My persistent pain condition
My persistent pain condition started eleven years ago, following a manual handling injury. I currently live with a permanently damaged sciatic nerve root which causes neuropathic pain, some back pain and a shoulder that intermittently causes me difficulties. As well as pain I experience other symptoms such as numbness and unusual leg/foot coldness, and I have an impaired ankle reflex and impaired balance.
Most of my pain and symptoms are neuropathic.
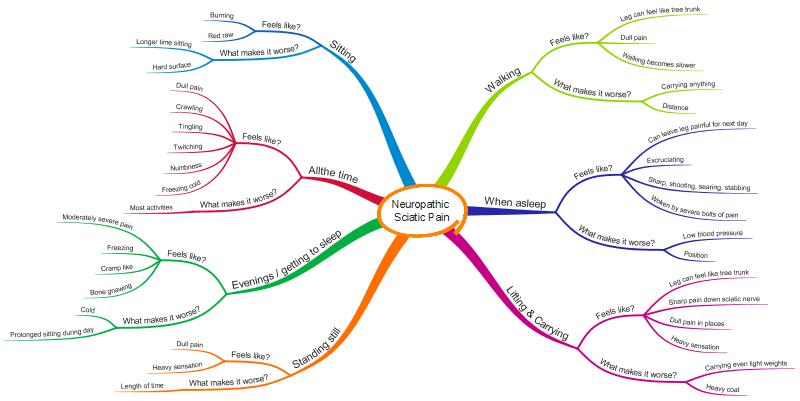
The following is a MindMap which illustrates how I personally experience neuropathic pain. Unfortunately I haven’t worked out a way of showing how often I have any of the symptoms, or how intensely I feel them, but hopefully it will give you an overall picture of how my neuropathic pain condition is experienced by me. Others will experience neuropathic pain differently.
Pain flares
I experience pain flares in two main forms, others will experience flares differently. My main type of flares relate to my neuropathic pain. However from time to time I also experience more generalised pain flares that might relate to my neuropathic pain and/or might relate to other vulnerable parts of my body, for example my back and/or my shoulder.
I describe these two different types of flares as ‘simple flares’ and ‘complex flares’.
Simple flares
For me ‘simple’ flares occur when I have excessively ‘wound up’ my sciatic nerve root over a period of time. The nerve root becomes increasingly aggravated, temperamental and ‘explosive’.

During a ‘simple’ flare I can expect to experience a week or more of daily multi-episodes of severe neuropathic pain, particularly during the evenings and sporadically through the night. I become more sensitive to experiencing pain, and overall I live with increased neuropathic pain and symptoms.
I describe these flares as ‘simple’ as it is my most common type of flare, and predominantly involves my neuropathic pain. Some other parts of my body may continue to be in pain at their ‘normal’ levels, for example my back, but it is just the neuropathic pain element that has particularly heightened.
These simple flares tend to happen for me if I am in a situation where I am sitting still for extensive periods, or worse standing still, doing any lifting and carrying (even relatively light things) or if I am overly stressed.
I can get away with doing these types of things ‘excessively’ for maybe two or three days without entering into a flare situation, but if I continue with them over a longer period then I can expect my condition to flare. Nothing is certain though.
Once I’m in a flare situation I usually have to work hard at reducing as many pain triggers as I can whilst my sciatic nerve root ‘winds down’ and ‘resets’. If I don’t start working at reducing the triggers then the flare will increase in intensity and take longer to calm down.
As well as reducing pain triggers, I do everything I can to positively improve my life, both during the flare and going forward. For example, I try to reduce any stress I’m under and do things that relax me and make me happy.
I find that once I enter a flare situation then my sleep is inevitably disturbed. For me this can cause a viscious cycle as lack of sleep can increase my pain levels, and then the increased pain levels can cause lack of sleep! In a flare I work hard to ensure the best sleep I can.
Emotionally any type of pain flare can take it’s toll. Even though I am used to living with persistent pain, any significant increase of pain, particularly if it affects my sleep for more than a night or two, can be hard going!
Thankfully my simple flares aren’t very long lasting, and emotionally I can usually bounce back from them relatively easily. Repeated simple flares cause me more difficulties, but I usually take a flare as a warning sign and adjust my life accordingly to avoid another in quick succession. I don’t always get this right though!
It is my ‘complex’ flares that I find the most difficult.
Complex flares
Like many other people I have more than one health condition. I think of a ‘complex’ flare as being when more than one of my conditions flare at the same time, or I experience a domino effect of flares. For example my neuropathic pain might flare, closely followed by my back pain flaring, and then maybe my shoulder pain flaring.

Thankfully complex flares are relatively rare for me.
In the past I have considered my shoulder condition to be completely separate from my sciatic nerve root and back condition, but I am now realising that all my ‘pain conditions’ are fundamentally connected.
It feels to me as though my sciatic nerve root, my back and my shoulder are in a state of equilibrium, and as one varies there can be an impact on the others.
In addition, sometimes my overall body pain sensitivity dial is turned up, maybe because I have been experiencing a simple flare of my neuropathic pain, which contributes to the overall picture.
I think the combination of the variability and sensitivity of my conditions and my pain sensitivity dial being turned up helps to lead to a complex flare.
It sometimes feels as though being in significant pain with one body part can trigger another body part to join the ‘pain party’, and so a complex flare starts.
I personally find complex flares the hardest to deal with, partly because they can be more intense in terms of pain, and partly because the pain may feel quite different to that which I’m used to on a day to day basis.
Because I live predominantly with neuropathic pain, and I am used to experiencing severe neuropathic pain, neuropathic pain has a familiarity to it for me. Experiencing acute shoulder pain, for example, is less familiar to me, and for some reason I find that lack of familiarity harder to deal with.
I find complex flares almost have a life of their own, and it can be hard to predict what will happen next with them. Once I have entered a complex flare situation I have to work quite hard to reduce my pain triggers, and improve my well-being, in order to calm the flare down and return to my ‘normal’ persistent pain state. This process usually takes much longer than for a ‘simple’ flare.
Recovering from pain flares
Everyone’s experience of pain flares is different, and everyone will approach their recovery from flares differently.
I think of recovering from a flare in four main parts.
- Firstly, I need to be able to cope day to day with the pain I’m experiencing during the flare (and for me particularly during the night).
- Secondly, I need to reduce the increased pain levels, and get back to a ‘normal’ pain state, as quickly as possible.
- Thirdly, I need to ensure my mental health doesn’t overly suffer, and I regain ‘resilience’ as quickly as possible.
- Fourthly, looking forward, I need to revisit my work commitments, my social commitments and my pain management strategies so that I avoid getting into a flare situation again for a while.

I don’t pretend to be an expert on recovering from flares. However, based on my personal experience, I suggest the following tips for recovering from a pain flare, which I hope may be useful.
My top twenty tips for recovering from a pain flare
- Recognise this is a flare. Flares can sometimes have a habit of creeping up on you.
- Briefly reflect on what might have contributed to the flare (it might help you avoid others in the future). Remember there are usually a number of causes contributing, and may include factors such as: physical triggers, emotions, sleep, weather, inflammation etc. Sometimes you won’t be able to work out a cause, and that’s fine.
- Don’t over-analyse what might have caused your flare. This isn’t helpful. If you can’t quickly tell what might have contributed to it then move on.
- Don’t blame yourself for getting into a flare. This isn’t helpful either, you just need to move forward.
- Don’t panic or catastrophise. It is easy to think the worst when in a flare. At the same time don’t ignore anything you think is different and wrong. If you are concerned about your condition, then seek advice from your GP or other involved clinicians.
- Tell your family and friends you are in flare and talk with them about how best they can support you, without removing your independence.
- Give yourself space to recover. Look at ways to reduce any work or social commitments you have. (Don’t reduce them all though otherwise you risk becoming isolated which won’t help).
- Be particularly careful about ‘pacing’. Your ‘pain sensitivity dial’ is likely turned up. Reduce as many ‘triggers’ to your pain as you can. Put in as many pain-management techniques as you can.
- Remember what you have been taught by your physiotherapist, pain clinic, or other professional about how to manage a flare situation. If you have written a flare ‘plan’ then find it and read it. Now is the time to put everything you have learnt into practice, even though now may feel like the time it is going to be the hardest.
- Consider whether increased use of medications may help for a short while. Think about which medications may be particularly helpful. (Make sure you have discussed with your GP or other clinicians though!)
- Do what you can to ensure you can sleep reasonably well. This may not be easy!
- Make sure you talk to others about how your flare is affecting you. This is particularly important if you think you are, or might be, becoming depressed.
- Consider reading blogs written by others with similar difficulties and consider connecting with groups on social media. Find the ‘right’ support for you.
- Look after your emotional and mental well-being. Be kind to yourself. Access family and friend support. Make space and time for going out to places you enjoy and doing things that make you feel relaxed and happy.
- Maintain as much independence as you can (eg dressing, getting food shopping), but don’t be afraid to ask for help. Understand and accept temporary limitations.
- Maintain as much physical movement as you can, without aggravating your condition.
- You may need to pause more strenuous exercise, such as going to the gym, swimming, cycling etc, depending on how you are affected. This might include physiotherapy exercises too. Restart as soon as you feel able. (You may need to seek professional advice as to what you should and shouldn’t do.)
- Look forward. Accept you are going through a temporary ‘blip’ but focus on your life beyond that. Where might you go for a holiday? Who might you like to go and visit? What book might you like to read next? Find things you want to do and start doing them.
- As you recover, take time to think about changes you might need to make to your life to help you stay out of a flare situation for longer. Do you need to try to change your work pattern to reduce the risk of flares? Do you need to review your use of medications? Can you improve your sleep? Is there an activity, for example swimming or walking, you could start doing regularly to improve your overall health? Do you need to take advice about any financial difficulties?
- And finally, at any point in your flare, do make sure you seek professional help if you feel you need to. This may be from your physiotherapist, your GP, or a range of other clinicians or professionals.
A PDF of my top twenty tips for recovering from a pain flare can be accessed by clicking HERE.
I hope the description I have given of my approach to ‘flares’ might help others living with persistent pain, particularly if they have neuropathic pain, to develop their own approach.
There is no ‘one-size fits all’. Each of us needs to work out our own way of managing our persistent pain or other long term condition, including flares. This is merely mine. I hope it may be helpful for others to read.
As always I am very interested to hear any thoughts and comments on this post.
I would like to acknowledge the help and support my physiotherapist @MattLowPT has given me. He has patiently, and compassionately, helped me to understand my persistent pain condition and has helped me to develop my pain management techniques.




