Last year I wrote a well received blog called ‘A patient’s understanding of persistent pain’. It can be accessed by clicking HERE. Since that time I have continued to learn both about my own personal persistent pain condition, and about persistent pain in general. These are my FURTHER thoughts on understanding persistent pain.
My diagnosis, my standard treatment pathway
I have an on-going diagnosis of right sided neuropathic leg pain. I have a ‘tethered’ sciatic nerve root, and experience some back pain. I live in persistent pain and have some associated numbness and nerve twitching. I have also had back surgery.
Does this all sound familiar?
There are thousands of people with my diagnosis, right? There are ‘standard’ ways of treating my condition that will work for me too, right? Or my condition is such that it can’t be treated and I just have to live with it like everyone else, right? Everyone with a similar diagnosis needs to be treated following the same pathway, right? With basically the same treatment, right?
So why when I was treated in a ‘conventional’ way, as if I was part of a homogeneous group of people, was my treatment not effective enough? Why when I was treated within a ‘medical model’ of care didn’t I make good progress? Why didn’t I learn to self-manage my condition effectively? Why did I find life so very difficult?
After all, research has shown that I should work hard to improve my core muscles, right? Then my back would become strong and recover, right? Research has shown that nerve block injections are effective, right? Research has shown that medications such as gabapentin or pregablin will reduce my neuropathic pain, right? Research has shown that back surgery is effective, right?
So why didn’t these things work well enough for me?
Becoming self aware
I have lived with persistent pain for eleven years. I’m not going to tell you this has been easy, because it hasn’t, but I do believe I have been able to make the most of my life, and that basically I have learnt to ‘Live Well with Pain’.
I have been lucky in that over the years I have been taught to become more self-aware; to understand my condition and how it affects me. I have been helped to gain some understanding of persistent pain, and I have been helped to understand some of the anatomical features of my condition. Most importantly I have been supported to learn how to self-manage my pain.
Once I started to become more self-aware of my condition, I began to notice that when I was stressed my pain would increase. If I sat on a hard surface my pain would increase. If I was happy and socialising with friends or family my pain would decrease. My experience of pain wasn’t constant, and it varied significantly depending on what was going on in my life. Very occasionally, maybe if I was standing up talking in front of a group of people, or taking a lead in a meeting, it might disappear altogether for a while.
It became obvious that there was much more to my experience of pain than could be explained by any physical tug on my tethered sciatic nerve root, or any rogue impulses from my damaged nerve. My anatomy alone did not explain my experience of pain.
Am I the same as others?
Talking to other people with a ‘similar’ diagnosis, I discovered that my experience of pain and my other symptoms was often quite different to theirs. There were similarities, but importantly there were differences too. None of us had the exact same pain experience, even though theoretically we had similar anatomical structures. None of us had the exact same triggers to pain, although there were some in common. Everybody’s experience was unique.
I learnt too that there were often wide differences between our abilities to cope with our condition and situation. I largely retained my independence, whilst others became dependent. I escaped becoming depressed, whilst others experienced long bouts of depression. My anxieties increased, whilst others remained calm.
I discovered that other people could take gabapentin, codeine and other medications without many side effects, whilst I was struggling badly with them. Why couldn’t I do the same?
I may have the same diagnosis as others, but I certainly don’t have the same experiences.
I’m not the same, I’m an individual

So what is it that is different about me? Is it just me that is different and everyone else with my diagnosis are a homogenous group that can be treated in the same way? Or is it actually that every patient is different and every patient needs to be looked at more carefully as an individual?
As well as helping me to understand more about the experience of pain, and about my own condition, NHS Consultant Physiotherapist Matt Low introduced me to the work of Rani Lil-Anjum. Rani is a philosopher working within the field of medical science. One of the main strands of her work is causation and dispositions. Rani has helped me to understand some of her work, which I’m extremely grateful for as it has helped me to better understand my own situation, and why my experience of my condition is quite different to that of other people with a similar diagnosis.
I am fundamentally a complex person, just like everyone else is. At conception I gained a mix of DNA from my mother and father. There is no-one else with exactly the same DNA pattern as me.
I don’t know what a foetus picks up from their mother’s emotions and circumstances whilst in the womb, but I’m guessing my development as an individual person started there. Throughout childhood I was exposed to a unique set of circumstances and experiences that continued to help shape the person I am today. My individuality has been shaped by both my genetics, and my experiences.
My mother had some difficulties with anxiety. I wonder if my own difficulties with anxiety are borne out of my experiences growing up in close proximity with her, or from my genetical makeup, or from some of the difficult experiences I have had in my own life? Or maybe all three?
There have been so many experiences, both positive and negative, in my life that have shaped who I am. Some in my childhood, some in my early adulthood, some much later, and some today and yesterday.
There is no-one in the world who has had the same experiences that I have. There is no-one with the exact same health that I have, or the exact same body. There is no one with the exact same social circumstances that I have.
I guess it’s no wonder that my experience of persistent pain is different to others.
Moving on from BioPsychoSocial
Many people talk about treating someone within a ‘BioPsychoSocial’ model, but I defy anyone to separate out the complexity of who I am, and in particular my persistent pain condition, into the three distinct areas of Biological, Psychological and Social. Where do the lines get drawn? Surely I’m just a person, and need to be considered ‘as a whole’.
It’s no good trying to treat just the anatomical basis of my persistent pain, or the psychological side of it, or that which arises from my social circumstances. Everything combines and overlaps. Treating one part of an artificially divided me doesn’t treat the complexity of the whole of me.
In the diagram below I have tried to depict some of the factors that might impact on a person’s presenting health. Historically these areas might have been split into three separate circles (Bio, Psycho and Social), but I am choosing to depict them simply as a range of factors that affect every human being.
I have avoided using a ‘body map’ type picture of a person, as I wanted to emphasise that the person is a human being, living in the real world.
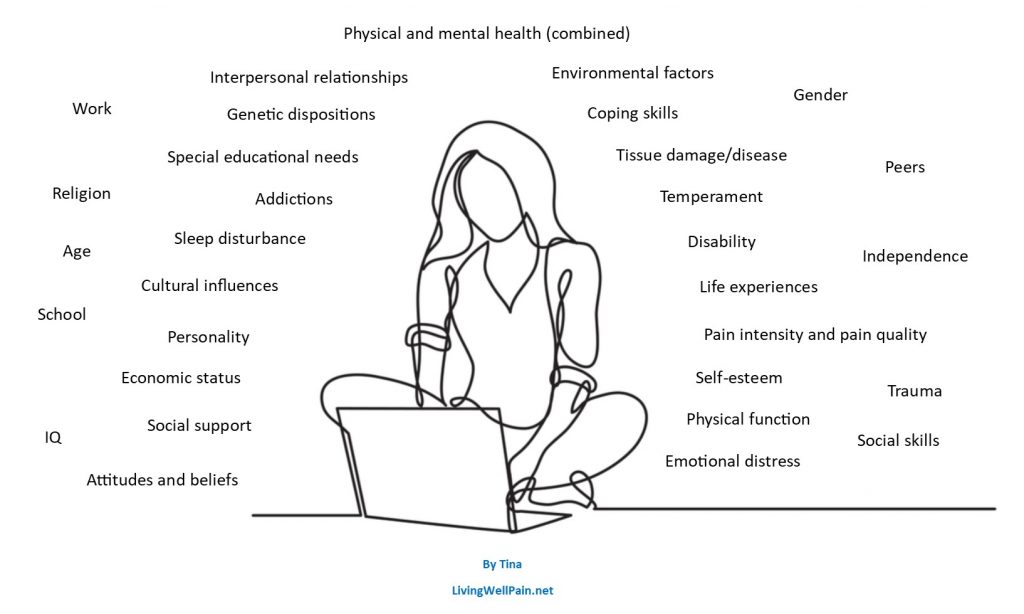
At first sight some of these factors might be thought of as being negative, whilst others positive. For example, I think it likely most people will initially think of ‘trauma’ as negative. However, for me trauma has had both a positive and negative impact on my life. As well as experiencing the inevitable negative emotions involved, I developed a great deal of resilience from being exposed to trauma at a relatively early age. I am sure this resilience has helped me cope with my persistent pain condition.
It is impossible to tell from a diagram such as this how each of these factors affect any individual person. It is only by listening to the person’s ‘story’ that you start to understand.
The 'causal' factors to my persistent pain
I have spent time considering what factors might be ‘causal’ to my experience of pain, and what my pre-dispositions, or dispositions, are. Just as I can’t separate myself out into ‘Bio’, ‘Psycho’ and ‘Social’, I also can’t separate out one factor as being completely distinct from another. They all interact and inter-relate. However in general terms I have been able to think through what might be significant contributing factors to my persistent pain condition.
The most obvious causal factor for me is my ‘damaged’ sciatic nerve root, and the ‘tethering’ with scar tissue that has occurred. My nerve root is ‘tethered’ to the disc it passes by, and also within itself. I have significant anatomical, mainly neuropathic, factors to my pain. However it is clear to me there are other factors too.

I have already indicated that it is impossible to properly ‘allocate’ a factor to being purely positive or negative. However, I have found it useful to think in simple terms about positive and negative contributing factors to my experience of pain. There will be times when one factor switches from being positive to negative and vice versa.
In simple terms, a positive contributor is likely to improve my experience of persistent pain, whilst a negative contributor is likely to make my pain experience worse.
There isn’t one positive or negative factor that will override all the others, not even my damaged sciatic nerve. I have a complex mix of factors that combine together. It is the particular mix of factors that in the end determines, in some way, whether I am likely to experience pain or not, at what severity level, and how much.
Of course some factors have more of an impact on the likelihood and severity of my experience of pain than others. The most obvious factor for me being my sciatic nerve impulses, but also, for example, if I were to experience really bad depressive symptoms, then I would almost certainly be more likely to experience increased pain.
For this reason, when thinking about the contributing factors (positive or negative) to my pain, I have also chosen to consider the intensity, or level, of those factors.
A year after my injury
The diagram below illustrates the factors that I think most impacted my persistent pain condition about a year after my injury occurred. The size of the text gives an indication of the intensity of the factor at that time, red text depicts negative factors and green text positive factors.
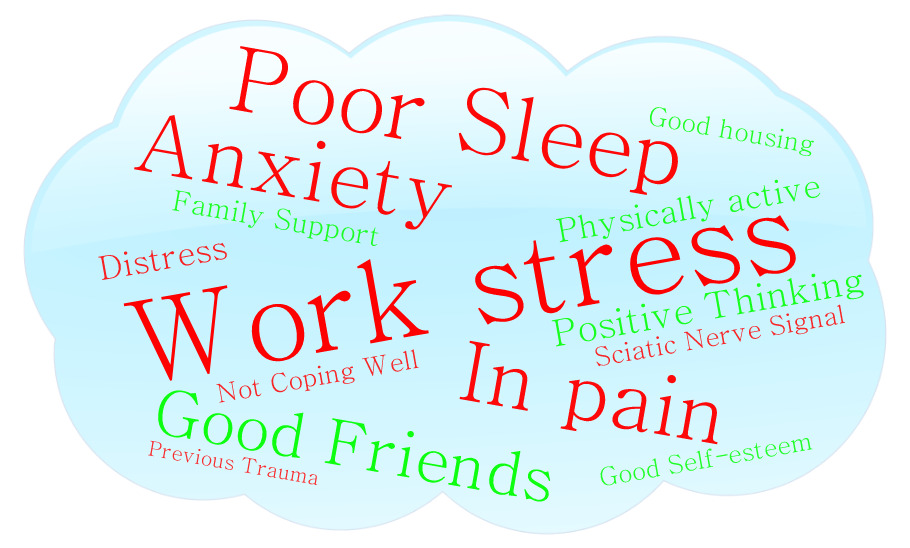
It is easy to see from this diagram that the particular mix of the causal factors is overall quite negative, and at this time my overall pain and distress was at a relatively high level.
There was significant interaction occuring between these causal factors. For example the more pain I was in then the worse my sleep was. The greater the stress I was experiencing at work, the worse my sleep and anxiety was. None of these factors can be viewed as separate entities, their interaction is complex.
I think the wordcloud diagram helps illustrate which areas of my life I could have tried to improve in order to support my overall persistent pain situation. Unfortunately I didn’t understand any of this at the time.
Being treated within the 'medical model'

Perhaps importantly the wordart diagram might have helped my clinicians realise they needed to provide a wider focus to my support and treatment than just my anatomy! In my opinion they needed to treat my anatomy AND help me understand the wide ranging factors to my experience of pain AND help me to learn to self-manage my pain. I needed to be treated within a person centred healthcare approach.
Following my injury, the first four years of my medical care unfortunately did focus only on my anatomy. I believe I was treated within a ‘medical model’ of care. Trying to improve only the anatomy of my body, which clearly couldn’t be ‘fixed’, was never going to fully address the complexity of my persistent pain!
If I could turn back time

I now know that I could have worked on reducing the negative contributors (red), particularly the stress I was experiencing at work and the difficulties I was having sleeping. I could have worked at bolstering some of the positive contributors (green), such as being physically active.
Just improving one factor on it’s own would have been unlikely to improve my overall situation sufficiently, I would have needed to work at improving a range of factors. If I had done this then I am sure that my persistent pain situation would have improved.
In those early days it would have been useful for me to have seen my pain situation depicted visually as a wordcloud in this way, and to have understood that there was more to my pain situation than the physical changes caused by my prolapsed disc.
Most importantly it would have been empowering to understand that there were things that I could do to improve my situation, without waiting for a surgeon to ‘fix’ anything, or for a medication to ‘cover up the pain’.
Wordclouds

I have spent some time trying to work out whether ‘Pain’ should actually be included in my wordcloud diagrams or not. After all ‘pain’ is the experience being derived from these causal factors and dispositions. However, there is no doubt in my mind that being in pain has a negative impact on everything, and that being in pain is likely to further increase my pain situation, so I left it in! I believe pain can become a causal factor in it’s own right!
My situation now
This next diagram looks at my situation now. I have kept the same range of causal factors for this diagram, in order to illustrate how they have changed. You can instantly see that the mix of factors is much more positive.
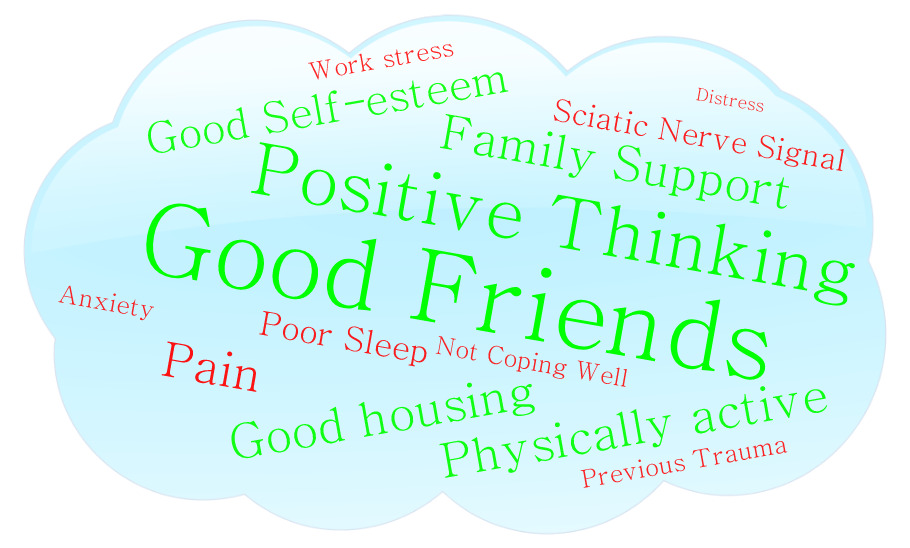
I’m not sure by how much my ‘anatomy’ is better than it was a number of years ago. My damaged sciatic nerve root still behaves badly, and I still have some back pain, but the effect this has on my overall life, and on my overall pain levels is much less. My anatomy alone does not dictate my levels of pain, and distress.
My pain journey turning point

The main turning point in my pain journey occurred when I was treated by NHS Consultant Physiotherapist Matt Low in a more holistic way. I was helped to understand the wider picture of my persistent pain condition, and I was helped to learn to self-manage my condition better. My persistent pain experience improved. This physiotherapy treatment occurred around four years after my injury, and I have written about it HERE.
Evidently I needed the wide range of my persistent pain causal factors to be considered within my treatment. I needed to personally understand how this range of factors, beyond my anatomy, might be contributing to my pain experience in order to start to be able to properly work on improving my condition myself.
Will the future be the same?

So now I understand my situation, and have learnt to self-manage my pain reasonably well, will my pain levels remain overall as they currently are for the rest of my life? I don’t think so!
I believe that if, for example, my work and social situation become more difficult, and my anxieties rise and my sleep becomes poorer, then my overall pain levels will increase, and I will be in a much worse pain situation overall.
I am working hard to avoid this happening!
Day to day variation

I think the two wordcloud diagrams above illustrate quite well how my overall persistent pain situation has changed over a period of years.
I do still experience variation in my overall pain levels month by month, and like many other people I also experience variation day to day, and sometimes minute by minute. The ‘rogue’ impulses from my sciatic nerve root are a strong influencer on my pain levels. I also experience ‘wind up’ of my neuropathic pain, which for me usually means I have more pain in the evenings than during the day.
I don’t yet fully understand the processes involved when my ‘tethered’ nerve is ‘tugged’, but I know this is a significant causal factor for me. I know that I can expect to experience maybe severe pain when my sciatic nerve is stretched, for example when getting out of the passenger side of my car on my steep drive.
I also know from experience that these more anatomical causal factors are only part of my picture. For example, if I am leading a training course then I am likely to experience less pain than I might otherwise expect to. The positive stress I experience, and the strong focus I would be providing to the course members changes my complex mix of causal factors, and changes my experience of pain. If my positive stress levels are particularly high, then quite often I don’t experience any pain. Luxury!
With the help of wordcloud diagrams, I have so far described how my experience of pain changes over large timescales. I hope now to explain how I think my pain experience changes within a short timescale, and in particular when I experience a strong input, or series of inputs, from my sciatic nerve.
A 'good' day
On one particular ‘good’ day my ‘background’ contributing factors might look like this, with my sciatic nerve root in a relatively ‘calm’ state.

As my sciatic nerve root becomes triggered, and starts to emit impulses, my complex mix of factors might change to something like this.

It is likely that this particular complex mix of causal factors and dispositions would mean that I experience some pain. The length of pain and the severity would depend on it’s particular composition.
A 'not so good' day
Perhaps on a different ‘not so good’ day my ‘background’ contributing factors might be more negative and look something like this. The sciatic nerve is in a relatively calm state here.

As my sciatic nerve root becomes triggered, and starts to emit impulses, my complex mix of factors might change to something like this.

The ‘background’ mix of complex factors was already quite negative, depicting a more difficult day in my life, but with the increase in my sciatic nerve impulses it is now even more negative. This predominantly negative mix of factors makes it more likely that I will experience pain, and probably quite a lot of it!
Predictive processing

My ‘background’ levels may vary day to day, or sometimes hour by hour or minute by minute. The complexity of this depends on so many factors, including my genetics, life experiences, natural dispositions, and what is going on during that period of my life, and in particular on that day! It is the complexity that is almost acting as a ‘predictor’ for my pain.
As well as learning a little about causation and dispositionalism, Matt has taught me a little about the role of predictive processing in pain. This has helped me to better understand how the nerve signals being generated from my nerve root, often spuriously, might be being processed in me to give me an experience of pain.
Fundamentally the predictive processing model of pain considers peripheral sensitisation, and looks at how anxiety, emotion, expectation and attention may change and impact pain. I have written a little about predictive processing within this article HERE.
Combining my thoughts on predictive processing, and causation and dispositionalism, and with the help of Matt, I have come up with the following description which has helped me to understand my pain.
A simple understanding of MY pain
I have in my mind/body a ‘model’ (predictive model) which informs me as to whether to give an experience of pain or not, in a variety of circumstances, based on presenting factors.
When a part of my body, in this case my damaged S1 nerve root (which may be being irritated by, for example, position, load or temperature), emits an ‘impulse’, then my predictive model considers this factor, along with other factors, to evaluate whether to give an experience of pain or not. These factors include my current novel mix of the levels of my traits.
I have a number of personal traits, or dispositions, which vary over time. For example, I have a tendency, or disposition, towards anxiety and poor sleep. I am naturally positive and have high resilience.
I experience interaction between these dispositions. For example, my sleep is likely to be worse when I am anxious, and my resilience is likely to be reduced when I am sleep deprived.
Some of these dispositions have a stronger influence than others on my presentation, for example anxiety and poor sleep have a greater impact on me than positivity.
I am also affected by external factors. For example, my anxiety will increase if I experience work place bullying or an unexpected household bill, and my positivity will increase whilst experiencing success.
I have an ever-changing novel mix of the levels of my dispositions. At a ‘good time’, my anxiety might be low, my positivity high and I might have had good sleep. At a ‘bad time’, my anxiety may be high, my resilience low and my sleep poor.
My predictive model ‘knows’ what combination of dispositional levels and other factors, including the impulse from my S1 nerve root, are likely to be ‘ok’ and don’t need a response of pain.
If the combination of factors at a moment in time, including the ‘impulse’ from my S1 nerve root (which is likely for me to be a dominant factor), matches the predictive model of being ‘ok’, then no action is taken, and no pain emerges.
If not, then pain emerges to alert me to do something to stop the irritation on the S1 nerve root continuing.
Changes in the novel mix of my dispositional levels, and my S1 nerve root impulse, may, or may not, be sufficient to change whether I experience pain or not.
My experiences inform my predictive model. These experiences might result in the predictive model being changed.
In order to improve my pain situation, then I would need to work on optimising my personal factors, eg anxiety, sleep, resilience and positivity, my physical factors, eg S1 nerve root irritation and also external factors, eg temperature, finances and work conditions. This is because my predictive model takes the combination of these factors into account when deciding whether to give me a pain experience following an impulse from my S1 nerve root. Improving one factor only is unlikely to bring about sufficient change.
Final thoughts
I hope this blog might support other people living with persistent pain to understand that there are many more factors involved in a persistent pain situation than just their anatomy. I hope this might help empower people to change the things they can change in order to improve their situation. Learning to self-manage persistent pain situation is not an easy journey, but a vitally important one. It truly changed my life!
In terms of physiotherapists and other clinicians I would make a final plea to listen to the ‘story’ of each of your unique and very individual patients.
Tina
@LivingWellPain
www.livingwellpain.net