It is now over fourteen years since I incurred a manual handling injury that was to change my life forever. My L5/S1 lumbar disc prolapsed, and I commenced a life of persistent pain and disability. Gone were the days I could walk freely, sit where I wanted, stand in queues, lift, and carry, and generally live without pain. Instead, sciatica moved in to accompany me for every second of every day for the rest of my life.
I guess I would have to characterise my sciatica as being at the more extreme end as for me it includes a strong element of neuropathic pain and numbness. I have been fortunate that gradually over the years my sciatica has improved, perhaps mainly due to skilled help from a physiotherapist, and some sheer hard work, but also due to the passage of time, natural healing, and the rejection of strong pain medications.
Following my manual handling injury, I was hospitalised for five days. I couldn’t walk, sit down, or stand. I was in excruciating pain and on high levels of pain medication including morphine. My life had been turned upside down. It took weeks before I could walk anything more than a few yards, and probably months before I could sit down for more than a few minutes. The neuropathic pain I was experiencing was severe.
I continued to live my life the best I could. The pain was causing me to constantly lean across to my left side, which I was aware of but couldn’t stop. I would do anything not to put any pressure on what I viewed as my injured leg.
Of course, it wasn’t actually my leg that was injured, rather a sciatic nerve root in my back, but even though I knew the truth of the situation it still FELT as though it was my leg that was the problem. That after all is where I FELT the pain and other sciatica symptoms.
Body perception disturbances
Whilst I could tell I was becoming very lopsided, I hadn’t realised that something else was going on. I hadn’t realised that in my mind I had ‘rejected’ my right leg and disconnected it from my mind’s body map. (For more information about a mind’s body map please follow the external links given at the end of this article.)
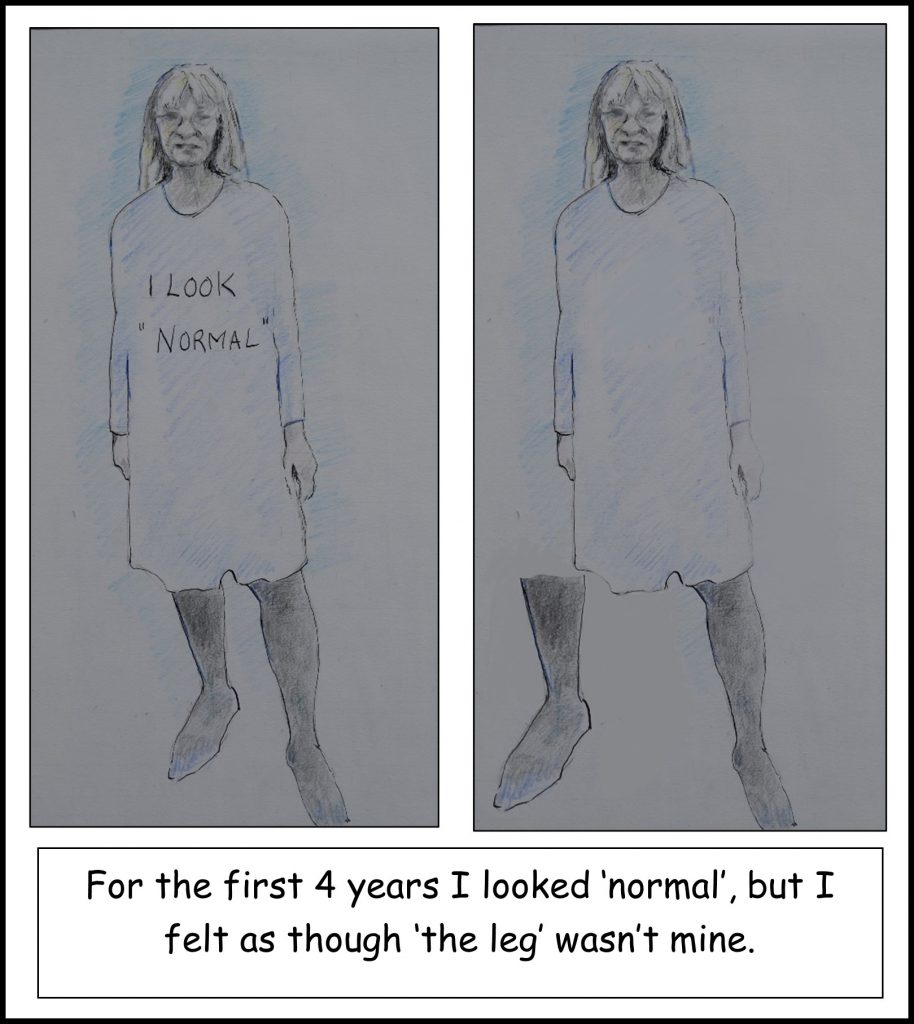
Consciously, if I looked down at my leg I knew it was mine, but subconsciously it was as though it belonged to someone else. I hadn’t realised that I no longer spoke about ‘my’ leg, but instead spoke of it as ‘the leg’, or ‘it’. There was a disconnect. In my mind ‘my’ leg wasn’t mine.
Looking back, I think it is understandable that this ‘disconnect’ or ‘body perception disturbance’ occurred. After all, literally overnight my leg had changed from one that felt just like the other to one that was totally alien, devastatingly painful and felt completely different. It just wasn’t ‘my’ leg anymore. It had changed my life, lost me my teaching career, and left me with extreme pain and disability.
I was perhaps fortunate that there wasn’t a complete disconnect. I understand that some people with body dysmorphia, or body perception disturbance, don’t even consciously recognise their body part as their own, let alone subconsciously, and some even want their body part to be removed by amputation. Nevertheless, there was a disconnect which needed to be recognised and addressed.
It was around four years after my injury that a skilled physiotherapist, Matt Low (@MattLowPT), picked up on the terminology I was using when describing my leg, and the way I was talking about it. He reflected to me that I was calling it ‘the leg’ or ‘it’ and described in simple terms to me about ‘disconnect’ and dysmorphia. I could immediately recognise that I was perceiving my leg as something that wasn’t really mine. I can still remember how it felt, as though it was in some strange way physically separate from my body, even though I knew it wasn’t!
Working with a talented artist, Anna Fraser from Exmoor, we recently created this picture of how it felt at that time
Treatment of Body Perception Disturbances
My physiotherapist talked to me about how I could start to resolve the problem. My memory is slightly fuzzy here, as he was also talking to me about ‘desensitisation’ at the time, and I can’t remember whether this ‘desensitisation’ related only to this body perception problem or another, but fundamentally he described that I needed to accept and make friends with my leg and re-integrate it properly back into my mind’s body map.
What followed was quite a lot of hard work on my part, extending over time. I can’t remember exactly how long it took to ‘reconnect’ my leg, but it was certainly weeks rather than days. I had to work hard at changing my mindset about my leg. Every time I caught myself calling my leg ‘it’ or ‘the leg’ I corrected myself. I spent many hours thinking about my leg and my accident, and I guess I went through another period of grieving for the life I had lost and acceptance of the life I now had. I had to stop ‘blaming’ my leg for what had happened and be grateful that I had a second leg to be able to stand and walk on.
As well as trying to change my emotions and conscious thoughts about my leg, I spent a lot of time looking at my leg, touching it and stroking it. I needed to ‘make friends’ with my leg again. I used different materials to touch my leg so that I could feel the different sensations, rough or smooth. I can remember doing these ‘exercises’ frequently through the day, for short periods of time, every day for maybe weeks. As well as doing these more ‘out of the ordinary’ activities, I spent time during my ‘normal’ day to day activities thinking about, and concentrating on, my leg and the sensations WE were experiencing. When I had a bath, I concentrated on how the warm water felt on my leg, when getting dressed I looked at my leg and consciously felt the clothes going on. I bought a variety of objects, massage oils and electrical devices, anything that would provide a different, and obvious, sensation to my leg.
Eventually over time my mindset changed towards my leg. It was no longer ‘it’ or ‘the leg’, or something to be blamed or resented, it just became ‘my leg’ once more. I had ‘made friends’ with my leg. Gone was the sensation that my leg was ‘disconnected’ and almost separate from my body. My mind’s body map had accepted my leg back into the fold.
Unfortunately for me it had taken four years before I met a clinician who recognised my body perception as a problem, discussed it with me and supported me to address it. Once I did it took a lot of hard work on my part to ‘re-connect’ my leg, but I strongly believe that every minute spent was worthwhile. I am sure that re-integrating my leg back into my mind’s body map has strongly supported my management of my sciatic condition, and my ability to live with it reasonably well. I now look favourably on my leg, and I now fundamentally want to ‘look after it’. I just cannot imagine what situation I would now be in if I had spent the last 14 years with a perpetual feeling that the leg wasn’t mine, and was at least in some way disconnected from my body. Those feelings couldn’t possibly have been helpful to me.
Summary
There is no doubt in my mind that during the first four years of my sciatica journey I had a significant problem with my body perception, and that my leg was somehow at least partially disconnected from my mind’s body map. That my leg just ‘wasn’t mine’.
For me it was hugely important that my initial body perception disturbances were recognised and treated. I am convinced that doing so significantly changed the course of my condition and my self-management of it. I would definitely recommend to anyone who thinks they have a problem with body perception disturbances to seek support and address it, and I would definitely recommend to clinicians that if you recognise this in one of your patients you do not turn a blind eye.
Further information
There appear to be several terms to describe problems related to the mind’s ‘body map’, but the terms I most identify with are body perception disturbances (or disorder) and body dysmorphia. Body perception disturbances seem to have mainly been studied in people with Chronic Regional Pain Syndrome (CRPS), but I’m not entirely sure why. I can completely identify with what is described for CRPS with my condition of sciatica. I’m sure body perception disturbances must be present in many other conditions also.
For those people who are interested in the more theoretical aspects of the body dysmorphia or body perception disturbances I have described, I have included some links to documents I have found helpful.
Body Perception Disturbances (BPD) in CRPS
Complex Regional Pain Syndrome in Adults 2nd edition
I am very happy to receive thoughts and comments on this post.
You can download a pdf copy of the blog: My leg isn’t mine.
Tina
@livingwellpain
www.livingwellpain.net










