Ten years ago, my life was changed by a manual handling accident. I now live in persistent pain, but I still live a good and fulfilled life, just one that is different. Before the accident, like everyone else, I experienced pain periodically, for example when I fell over, when I sprained my ankle or when I burnt myself on a hot pan. I assumed that pain meant I had physically ‘hurt’ a part of myself and that when it ‘healed’ the pain would stop. I didn’t put much thought into what pain was or what it was affected by. I didn’t need to.
For the first four years after my accident I remained largely ignorant of what causes pain and the factors that contribute to the experience of pain, for example stress, difficult family relationships or trauma. I was experiencing daily pain, and medical interventions were not sufficiently helping me. I had experienced several episodes of physiotherapy care but despite this, and other medical input, I did not understand pain and what might be done to ease persistent pain.
Around four years after my accident I had an episode of care undertaken by Consultant Physiotherapist Matt Low, and it was through this that I started my journey of understanding pain. I have written about that episode of care, which followed a Cognitive Functional Therapy approach, and for me was life changing, HERE.
As well as explanations from Matt, I started to learn about pain by reading ‘Explain Pain’ by Lorimer Moseley and David Butler. Understanding more about pain was hugely important to me in terms of understanding my own condition and better managing it. With Matt’s help my new understanding enabled me to put into practice better pain management, which I have written about HERE.
However, Explain Pain wasn’t enough for me to fully understand MY pain. It was a good start, but I struggled to completely fit my own pain situation into the descriptions given. I needed a better understanding.
My long journey to sufficiently understand MY pain has at times been rocky, and to be honest at times emotional. I have struggled to fit MY experience of pain into the various models and explanations put forward and have only recently, again with the help of Matt, come to an understanding of pain that I think fits with MY experience of pain, and which therefore I can ‘buy into’ and move forward with. I hope that this better understanding of pain will help me be able to further improve my life with pain. I think it will.
My pain
At this point I think it would be helpful to give a brief description of my pain situation. I hope this will help to start to explain why I have found it difficult to fit my pain experience in with some of the models and explanations of pain put forward.
My pain follows a manual handling accident ten years ago, in which a herniated disc damaged my sciatic nerve. I underwent back surgery eighteen months later, but the nerve damage proved permanent. I have been on a long journey of rehabilitation and ‘recovery’. At the start I was basically unable to walk, sit and was in constant severe pain. I have quite gradually improved over the years.
For many years following my accident I experienced significant back pain and significant neuropathic pain. I currently experience mainly neuropathic pain with some back pain. I think it is my experience of neuropathic pain that has made it particularly difficult for me to fit my personal pain experiences in with the pain explanations put forward by others.
Rather than writing a blow by blow account of my pain and how it currently affects me, I have created a MindMap below. As it is the neuropathic pain which currently has the largest impact on my life, and which has caused me the most problems when understanding pain, I have only included that part of my pain.
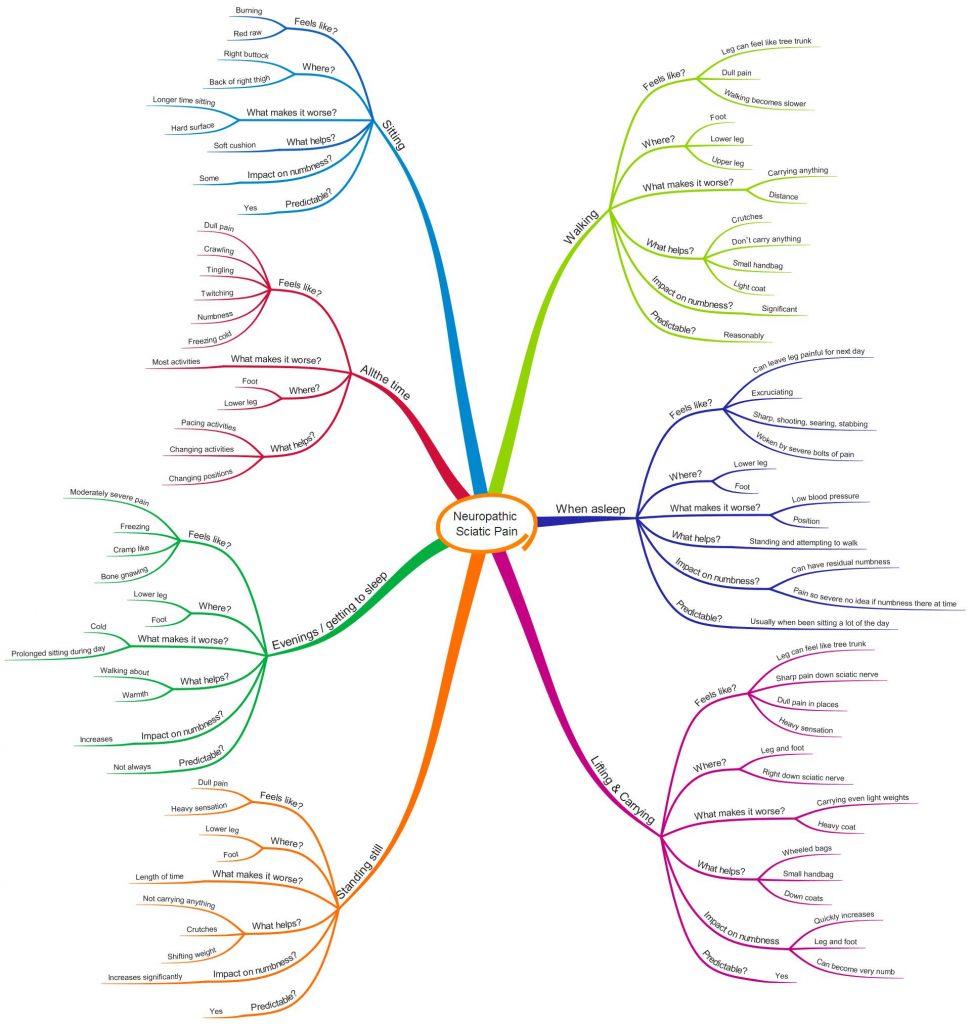
Unfortunately, you can’t tell from the MindMap how much pain I have, or how often I get each of the symptoms. I can’t yet think of an easy way to show this.
My difficulty with pain explanations
I need to start this section by saying that although I personally have some difficulties with some of the published explanations of pain, and some of the analogies used, this does not mean that they aren’t useful for other people. Everyone’s experience of pain is different, as are their learning styles, and ways of thinking. When I was teaching I often used to have to explain things in a totally different way to one child than another.
When you live in pain and you read something about how pain works you try to fit your personal pain experiences into what you are reading, or at least I do, and when you just can’t fit your experience in then this can lead to confusion, frustration and despair, or at least it has for me.
Several books, articles and videos explain that your brain makes pain when it concludes your body tissues are in ‘danger’ or under ‘threat’ and you need to do something about it. I have found the concept of ‘danger’ or ‘threat’ to be too extreme for me. I haven’t been able to reconcile this with my experience of pain. For example, when I am sitting down my sciatic nerve becomes irritated and will produce pain. As far as I’m concerned, no part of me is in ‘danger’. The concept of ‘danger’ just doesn’t make sense to me for most of my pain.
I fully understand that there are psycho-social factors related to the experience of pain, and to be honest this was probably the most important new learning for me when I started to learn about pain, but for me some of the explanations of pain seem to over-emphasise the psycho-social factors, and hardly mention bio factors, again causing me to have a mis-match between my pain experience and what I am reading.
I have a damaged sciatic nerve which is an important, and I think dominant, factor in my experience of pain. Like everybody else, my psycho-social factors vary from day to day, and to some extent vary within each day, and I am sure affect my overall experience of pain. However, when I think about, for example, the severe bolts of pain I experience when I am asleep, I find it difficult to rationalise that pain experience with explanations of pain that emphasise the psycho-social factors way above bio factors. I know from experience that there is a strong link between the severe pain I experience during the night and the amount of sitting I have done during the day (and therefore physical irritation of the sciatic nerve) but only a weak link, if any, to my day to day psycho-social variance. Having such a strong emphasis on psycho-social factors in explanations of pain, and often very little mention of bio factors just doesn’t make sense to me for my nerve pain situation. It creates a mis-match between my pain experience and what I am reading.
Another diffficulty I have had with common pain explanations is with the idea that ‘pain doesn’t equal damage’. Although I have in loose terms found this idea helpful, I have had to re-formulate it in my mind to ‘pain doesn’t equal MORE damage’. If my sciatic nerve had never been damaged, then I wouldn’t be experiencing sciatic nerve pain, and so of course to me my pain is directly linked to my nerve damage, and always will be.
I have also experienced difficulties with published explanations of pain when they have said that anyone can overcome pain and lead a pain free life. I believe my sciatic nerve to be permanently damaged, and likely to cause me pain for life. I may be able to manage that pain, and hopefully reduce it, but unless someone can convince me otherwise I don’t believe that improving my life in terms of psycho-social factors, or ‘turning down the pain volume control’ is going to enable me to live pain free. Obviously, I hope I’m wrong in this belief, but this has caused another mismatch between my pain experience and what I have read. This mismatch has caused me confusion, and on occasions distress.
I have desperately wanted to fit my experience of pain into the frequently put forward explanations of pain, but they just don’t work for me, certainly not in their entirety.
I have a strong personal need to understand my pain enough such that I can use that understanding to work out further ways forward with my pain, and, to put it bluntly, to stop being knocked sideways every time I read an explanation of pain that just doesn’t match my personal pain experience. I have therefore looked, again with the help of Matt, at the more recent thinking behind pain.
MY understanding of MY pain, based on the Predictive Processing Model, the Mature Organism Model and Dispositionalism
My improved understanding of MY pain is based on the Predictive Processing Model, the Mature Organism Model and Dispositionalism. I’m not a clinician, or a pain scientist, or a philosopher, and so I’m not intending to try to explain these models here. The following links can be used to reference the main articles that informed my thinking (combined with input from physiotherapist Matt Low). I’ve also watched some YouTube videos of Mick Thacker and Matt Low presenting information about these topics and included those links.
The use of dispositions in clinical practice
Mick Thacker – Cause Health – 12th May 2016
Matt Low – Cause Health – 12th May 2016
Interestingly with these models I have been able to fit MY pain experience into the explanations put forward without undue difficulty.
Based on these models, I have created for myself a simple understanding of what happens with MY neuropathic pain. I think this simple explanation works with my non-neuropathic pain also, obviously slightly adapted to change the words ‘sciatic nerve’ for others.
My simple understanding of my pain:
I have in my mind/body a ‘model’ (predictive model) which I use to decide whether to give an experience of pain or not, in a variety of circumstances, based on presenting factors.
When a part of my body, in this case my damaged sciatic nerve (which may be being irritated by, for example, position, load or temperature), emits an ‘impulse’, then my predictive model considers this factor, along with other factors, to decide whether to give an experience of pain or not.
As well as the ‘impulse’ from the sciatic nerve, factors include my thoughts, feelings, beliefs, past experience with sciatic nerve, life experiences etc. Other factors might be, for example, environmental temperature, stress, tiredness and how irritated the nerve has been during the day.
My predictive model ‘knows’ what combination of factors are likely to be ‘ok’ and don’t need a response of pain.
If the combination of factors at that moment in time, including the ‘impulse’ from my sciatic nerve, matches the predictive model of being ‘ok’, then no action is taken, and no pain is produced.
If not, then pain is produced to alert me to do something to stop the irritation on the sciatic nerve continuing.
My predictive model changes with my experiences and is constantly being updated.
My predictive processing analogy
I like analogies to help understand difficult concepts. I wanted to find an already produced analogy for the predictive processing model of pain but was unable to. I couldn’t find any patient friendly material about the predictive processing model, and I’m not sure if this is because I just don’t know where to look, or because the model is new, still under development, and nothing patient friendly has been written about it yet.
As it is currently important to me personally to come up with an understanding of pain that I can live by for at least the next few years (until pain science moves forward again), and as the subject is complex, I have come up with the following analogy to help me remember and understand.

I have a fourteen-year-old daughter, Amy. She is a lovely girl and likes to go out with her friends. She has just asked me if she can go for a sleepover with her friend Tasha. I must decide whether to let her go, and if I decide no, how firmly I’m going to need to tell her. Part of my decision will be about how safe I think the situation will be for her.
Amy has been on sleepovers before, as did I when I was her age, so I already have in my mind a ‘model’, or ‘picture’, of what sleepovers entail. I also have an idea of how flexible I might be around my decision. I have an ‘expectation’ of what an ‘ok’ sleepover would be. I have ‘prior’ thoughts and feelings around this. For example, if Amy asks me to have a sleepover with a boy then I’m likely to say no, if her friend’s parents won’t be there I’ll likely say no, but otherwise I might be ok with it, depending on what else is going on for me at the time, and what else she tells me.
I am only human, and my response to Amy is going to be affected by several factors other than whose house she is going to and who with. For example, I’m a slightly anxious person, and my decision may be influenced by how anxious I may be feeling on that day. Amy may have been annoying me and winding me up all day, which will likely affect my decision. I might be stressed at work, which may make it less likely I’ll agree, or I might be happy due to a work promotion which may make it more likely. My decision might be affected, either consciously or sub-consciously, by something that happened to me as a child when on a sleepover. There could be snow outside which might make it less likely I’ll agree.
To decide whether this sleepover would be ‘ok’ or not, I use the model in my mind to compare my expectations of what would make up an ‘ok’ sleepover with all the presenting factors, for example those mentioned above. The request from Amy is likely the main factor, but my decision is going to be affected by lots of other factors.
I decided to let Amy go on her sleepover.
I find out later from one of Amy’s friends that Tasha had been plying her with alcohol and offered her drugs. Inevitably this altered the model in my mind around sleepovers, and what would be ok to agree for Amy in the future. I will be less likely to agree to a sleepover, especially with Tasha, and more likely to say no.
Shortly after this, Amy asked me if she could go on a sleepover with Tasha. I compared my new model of expectations of what an ‘ok’ sleepover might look like with the presenting factors. The strongest presenting factor in this case was the choice of friend, Tasha, but there were others, for example I had had a good day with Amy. I decided to say no to Amy’s request, in fact I shouted this at her. I wanted her to understand that this was something she really mustn’t do.
The following day, Amy asked me if she could go on a sleepover with another friend, Ella. I compared my new model of expectations of what an ‘ok’ sleepover might look like with the presenting factors. In addition to other factors, Amy had been annoying me and winding me up all day, I was tired, and I was experiencing moderately high levels of stress and anxiety. I decided to say no, but I did so in a less aggressive way. I didn’t feel the need to be quite so strong with my response.
The next week Amy asked if she could go on a sleepover with Ella. I compared my new model of expectations of what an ‘ok’ sleepover might look like with the presenting factors. This time I wasn’t so stressed, and Amy had been behaving well. Considering these, and other presenting factors, I reasoned that this sleepover would meet my new model of expectations of being an ‘ok’ sleepover and so I allowed her to go.
This turned out to be a successful sleepover. I updated my model of expectations of what an ‘ok’ sleepover might look like, ready for the next request.
Hopefully this analogy also makes sense to others. Fundamentally instead of a decision about a sleepover, my mind/body is making decisions about whether to give me an experience of pain, and if so how strong an experience of pain that will be. Like the analogy this decision is based on a range of factors, including an impulse from the sciatic nerve (the request for the sleepover) and a range of psycho-social factors, and possibly other bio factors. Although I think the analogy works for all my pain experiences, it was initially written based on my neuropathic pain experience, hence the reference to ‘winding up’ (I think you can get ‘wind up’ of all pain though?). The psycho-social factors that influenced my decision about a sleepover, are similar factors to that related to my experience of pain.
Understanding pain has been hugely important to me in terms of my learning to manage my pain situation and lead as full and fulfilled a life as possible. Having a narrative in my head about what is likely affecting my pain and what is happening with my body, which I can fully identify with is hugely important to me, and I’m sure others. It provides me with the confidence to try different things, cope when I am experiencing a flare of symptoms, work out different ways of doing things in order not to ‘wind up’ my condition and generally live well despite living in pain.
I am grateful to everyone who has helped me come to an understanding of my pain that I can now fully buy into (at least for the moment until science moves on), but obviously particularly to Matt Low who has shown endless patience in his support of my need to understand MY pain. I wish to also acknowledge the support Matt Low has given to me in writing this post.
I look forward to watching progress with the Predictive Processing Model, and with Dispositionalisms. Interesting times.
I am very happy to receive thoughts and comments on this post.
Tina
@livingwellpain
www.livingwellpain.net











Thank you for this post a very informative read. Question…..how do you know you have a damaged sciatic nerve?
Hi Adrian
Thank you for your kind words.
I’ve had quite a lot of medical investigations, and I’m told by clinicians I trust that my nerve is damaged.
Tina
Have you challenged the assumption that your sciatic nerve is actually “damaged”? A lot of times doctors will make relevance out of an MRI or EMG. Can you do 20 calf raises on your right and left legs without an issue?
FYI, I recommend reading a book called “A world of hurt: A guide to pain classifying pain” and checking out a guy named “Craig Liebenson”. It may (or may not) help.
Hi Tina!
Beautiful writing!
I am physiotherapist, with experience in chronic pain and specialized in neurological rehabilitation. I have to give you a big thank you for your text.
Can I give you some ideas?
– The discomfort we feel when we are in the same position for too long. We can’t ignore this. And this is important. If we ignore, in extreme circumstances we can damage tissue (like pressure ulcer). This is extreme, ok, and it will not normally happen unless when we have a prior problem of sensibility. But it is to illustrate the fact that we use that kind of information for protection.
I usually use the allegory of a really long bus trip, and we can’t move… Horrible :p
– Normally, in neuropathic pain, I use lots of prevention exercises: if your leg is “healthier” (in the point of view of the cardiovascular sistem), the pain may arrived but maybe later (“probabilistic” speaking). (See this with you physical therapist)
– In the final fase of the treatment I like to work with my patients this: make some piece with the pain, it’s useful, for body/mind have some perception about what’s going on. It’s like “don’t kill the messenger”.
What do you think?
(sorry for my English)
Big hug from Portugal,
Maria João Bigode
briliiant post for me as a physiotherapist to help my patients.
but how do you know that the falre up in your symptoms is caused by what? bio(too musch sitting) or psycho(stress or anxious) or social(bad day of work). ?
Thank you so much for your kind comments.
I’m not sure I can always tell what the causes of any increase in my symptoms are, but I’ve got 10 years experience of my condition now which undoubtedly helps. My symptoms change frequently during the day, every day, so interestingly I don’t usually talk about a ‘flare’ of symptoms, it’s just part of my daily life.
Thank you again
Tina
Hi
This really chimed with me. I live with chronic fatigue and have tried fitting myself into the medical boxes provided. Your post has given me the motivation and confidence to keep looking and discovering until I find an explanation that truly makes sense to me. When you live with something every day it is the very least you need. Thank you for helping me in my journey.
Abi
Hi Abi
Yes, I really do recommend you keep looking for the explanation that truly makes sense to you. I am so much happier now I have an explanation that makes sense to me. Might seem daft to others who haven’t experienced a similar situation, but to me it has been hugely important. I hope you find the explanation that works well for you soon.
Tina
Excellent post. I have a damaged pudendal nerve (from surgery) and also struggle to fit my pain into the medical models. I understand that the pain response comes from my brain, but I believe that every stretch or compression of that irritated, angry, damaged nerve creates a very real pain signal. There is a direct correlation between certain movements, general activity levels and my pain levels. Completely understand the wind-up factor caused by stress, emotions and fatigue. All very real contributors to the big picture. Your article helped me put it all in perspective. Wish I could get a medical opinion on my ‘model’.
Thank you Sue.
It’s good to hear from someone else who has an irritable nerve. I was lucky in that I had an amazing physiotherapist who understands pain very well and could explain it to me. He had to be very patient with me! I think it’s worth investigating in your area to see if you can find your own amazing clinician.
Glad the article helped.
Tina
Great post, thank you for sharing your experience and thought processes with us.
Thank you Maria. This was a heartfelt post for me!
Tina
Great post! I’m a clinician, and of course what we do to help patients doesn’t always work, so I’m looking for good educational resources to share for those who have to live with persistent pain. I too have struggled with simplistic accounts that suggest that all chronic pain is related to hypervigilance and trauma. I like the way you express your ideas clearly,
Thanks for being a great resource
Wishing you all the best
Miranda
Thank you, glad to hear others have similar thoughts!