In order to live the best possible life that I can with chronic pain, it was, and still is, important for me to learn how to manage my pain on a daily basis. Everyone’s pain is different, even if they suffer from the same medical condition, and each individual must work out pain management methods that work for them, preferably with the support of professionals. This is my approach.
What is pain management
When a baby is born they start to make sense of their own body and the world. They need to slowly learn, with help from their caregivers, what causes them pain, and learn how to avoid it. For example, they will learn not to put their hands on a hot radiator, not to put their fingers in a closing door, and not to bite their own hand. They must also slowly learn what makes them feel comfortable, and what makes them feel less comfortable. For example they learn about wearing warm clothes when it is cold, and the discomfort of a wet nappy. It takes a surprisingly long time for a young child to make sense of their bodies and learn how best to respond to them and look after them.
After my accident I was left with a body that works in a different way than before. Parts of it are malfunctioning and not behaving in the way I had previously experienced. For example my sciatic nerve is, in simple terms, mis-firing and my brain is mis-interpreting information being sent from it. For example, if my affected foot stands on a cold surface then the signals sent by my sciatic nerve are often interpreted by my brain as pain as well as cold. My pain mechanisms have gone haywire!
(Pain is hugely complicated in the way it works in the brain and body, particularly with someone experiencing chronic pain, but I want to avoid the complex scientific theories about this and so have stuck with a simplistic view here, from a patients perspective.)
I had entered a new world of chronic pain and just like a young child I had to learn about my new body, and how to avoid increasing the pain, and how to make myself more comfortable and with less pain. This, as far as I’m concerned, is what pain management is all about.
Sounds simple doesn’t it? Trust me it’s not, and for me it took a long time to learn to understand the changes in my body and how best to reduce the pain enough to cope with it day to day, and be able to lead a fulfilling life despite chronic pain. I was fortunate to have some amazing professional help in this process, however pain management is individual to each person and is something I had to pro-actively learn and develop for myself; it is my body and no-one else can experience the pain sensations that I do.
Recognising the pain triggers
Before I could develop pain management methods, I first had to recognise what was triggering the malfunctioning pain for me. Sounds simple doesn’t it? It’s not! For example, you would think that if I experienced a sudden shooting pain down my sciatic nerve, then I would be able to think about what I had done a few seconds before and that it would be obvious what had caused the pain, much like when I was a young child and I put my hand on the hot radiator. Unfortunately chronic pain doesn’t seem to work like that. Sometimes it’s obvious what has caused the pain, but often you have to be a detective over time in order to work out what the triggers for the pain actually are.
This isn’t helped by the ‘wind-up’ process of pain. In simple terms this means that, for example, if I sit for extended periods during the day, particularly if I sit on a hard surface, then this ‘irritates’ my sciatic nerve and ‘winds it up’ (much like a young child ‘winding up’ their mother through constant irritations). The overall pain will then intensify, mainly during the evening and night, and I may experience severe pain in my leg and foot. This severe pain will often include an ‘electric shock’ type of pain traversing my leg and foot. At the instant that occurs the pain appears to come from nowhere and it was only with careful thought over time that I was able to realise that it was what I was doing during the day that was affecting the pain I experienced later on.
Medications also complicate the ability to recognise pain triggers. I am very sensitive to medications, and to put it bluntly they make me feel quite ill with a variety of side effects. I was put on a range of pain medications immediately following the accident, and remained on a number for a few years afterwards. Learning about my new body and how to recognise pain triggers, and then how to minimise them, was hampered by the interplay of the side effects of medication. It was only when I stopped taking all medications that I could truly work out what was going on with my body in terms of chronic pain.
Pain triggers are not always easy to work out, but slowly identifying them is a process well worth going through as once you understand them you can start to pro-actively work out how to avoid them.
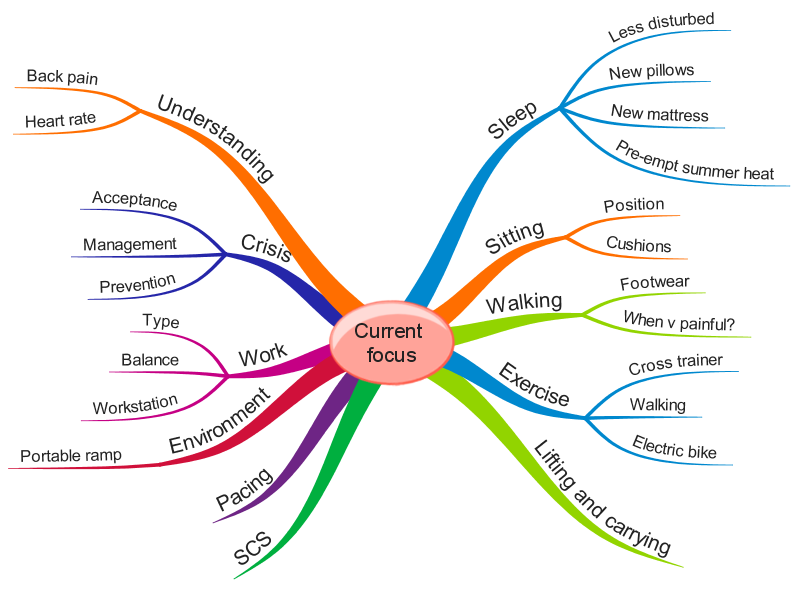
The following is the mindmap that I drew a number of years ago when I first started to address my pain management with the help of physiotherapist Matt Low, who used a Cognitive Functional Approach with me. It shows my pain triggers. For me, as with many others, that pain may be immediate, or may occur later during the evening or night. The more triggers I experience during any particular day the more likely I am to experience severe or prolonged pain. If I’m reckless and don’t actively manage the pain over a few days then the overall level of pain increases substantially. I can never get rid of the pain, but with pain management techniques I can improve it.

Interestingly, re-visiting this MindMap 5 years later, the pain triggers are basically the same. I am finding my pain condition to be more manageable now through the understanding of these triggers and through active pain management processes to mitigate against them. Obviously you will see I can’t fully mitigate against these triggers – I do have to sit down at some points during the day!
As well as helping me think through the triggers to my pain, I was able to use this diagram to talk through these triggers with my healthcare team. I certainly wouldn’t be able to remember all those triggers if asked in a hospital appointment, but writing them down helped the professionals to understand what was happening with me and support me work out the pain management techniques I needed to use.
Avoiding/mitigating against the pain triggers
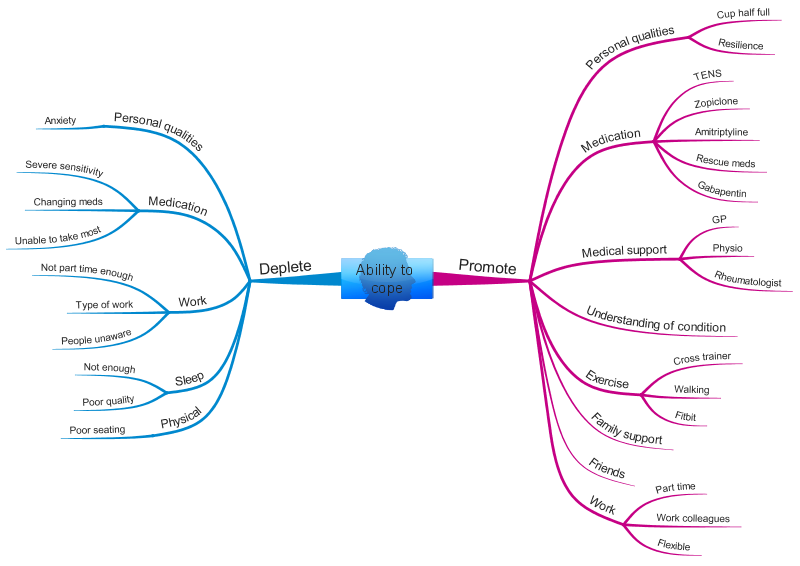
The next stage in the process was to think through and work out what I could do to reduce these triggers, and the resultant pain. The following MindMap shows my thoughts on this:

You can see that I carefully thought through what the difficulty with each pain trigger was, and how I could go about, for example, adapting my work pattern, my home or garden or my pattern of movement during the day. There are a lot of elements to this MindMap and it demonstrates how comprehensive pain management can be. A lot of these things I now do as a matter of course, but when I was first working all this out I had to prioritise elements and work on them a few at a time.
This diagram shows my priorities at a particular moment in time:
Other factors impacting on pain
Additionally I came up with a MindMap (below) which detailed an overall understanding of what made my pain situation worse, and what improved it, and in particular considered my ability to cope with the pain. For example, poor sleep had a negative impact on my overall pain levels, whilst exercise had a positive impact. Poor sleep is a common problem with those suffering chronic pain. I have been able to improve mine to some extent through good sleep hygiene.
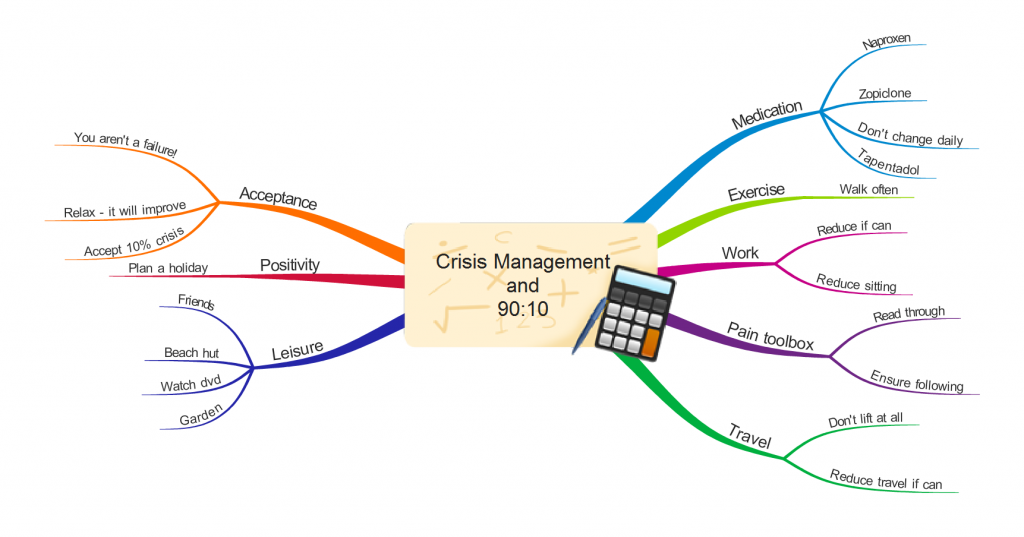
In times of crisis
Inevitably there were times that I felt ‘in crisis’ with the pain. I looked at my overall situation as ’90:10′, that is 90% able to cope with my pain situation, and 10% experiencing much more difficulty and ‘in crisis’. On reflection I think this is a fairly crude way of looking at the situation, but at the time it worked for me. Most importantly I put advance thought into what I should do when experiencing a crisis situation, which I sketched out in the form of the MindMap below. When experiencing a crisis I got the MindMap out and made myself start addressing some of the components! Once in crisis I think it becomes harder to pro-actively utilise pain management methods, which is unfortunate as this is the time you need them most!
Summary
Although I couldn’t, and can’t, get rid of my chronic pain, through careful thought, and to be honest sheer hard work, I have been able to learn to understand what affects my pain from both external factors (eg cold and lifting) and internal factors (eg stress). Armed with that understanding I have been able to adapt my life and environment in order to minimise the pain and facilitate me coping with my situation and leading a fulfilling life, including being able to work part time.
Using MindMaps to help think things through is an approach that works for me, others undertake similar analysis in different ways. It doesn’t matter what way you undertake this process, it just matters that you do it!
Tina
@livingwellpain
www.livingwellpain.net





Very interesting article. Thank you. Great to read something in patient speak. I am interested in your experience of the need to avoid triggers. Much of my reading on pain management, in particular John Sarno’s work says that we must stop avoiding that which we think triggers pain. Also my understanding is that if you do something and anticipate latent pain as a result your brain will produce it. I am at the point in my journey where I need to start doing something more physical. Walking triggers my pain ( any amount) but I can’t not walk for the rest of my life. Hope this makes sense!
Hi Siobhan
Thank you for your kind comments.
I totally understand what you are saying about avoiding or not avoiding triggers. I think it’s a balance. I definately ignore a lot of pain in order to lead as normal a life as I can, but I’m careful not to aggravate my condition when I don’t need to. It’s hard to get it right isn’t it?
You might be interested in reading this: https://livingwellpain.net/a-persistent-pain-acceptance-conundrum/ I too have grappled with the problem that accepting, and therefore anticipating, pain might lead to increased pain (hope that makes sense).
Thank you for the reference to John Sarno. Will read up about his work.
With best wishes
Tina
A very good and informative blog on pain management. Thanks for posting.
Thank you 🙏🙏🙏