Important Note
I feel it is important for me to say that these are my personal thoughts only, based on my personal experience of early trauma and my personal persistent pain condition. My thoughts are in no way meant to undermine the superb work that is being done with people who have experienced early trauma and who also experience persistent pain. I am a strong believer in trauma informed care, both in healthcare, social work, education and the criminal justice system. My point is that words matter, biases matter and good therapeutic alliances matter. Most importantly good person-centred, evidence-based, healthcare matters.
This letter is written to a combination of clinicians and clinical researchers/authors that have had an impact on me, either positively or negatively. It is not about any one person. It more likely covers 20 – 30!
I hope it proves helpful to hear this personal view.
My thoughts on what I would like for my future trauma informed persistent pain healthcare have been written HERE.
Dear Clinician
Do you remember me? I remember you. I first met you in a pain clinic when you asked me to complete a questionnaire before entering your room. I’ve since met you a number of times. I’ve even read your articles and research papers. I wonder if you remember me?
I first came to you in a great deal of pain and difficulty. Less than a year before I had experienced a manual handling injury, prolapsing a disc. I had been hospitalised for five days and I remained in excruciating pain. I was struggling to cope with the severe neuropathic and back pain I was experiencing. I could barely sit down and could barely walk.
I sat in your waiting room nervously waiting for my appointment with you. I was desperate for help. Your receptionist came out to me and asked me to complete some forms before coming in to see you. I was told that you made everyone you saw fill them in. I set about completing them. I wondered how they were going to help and what was going to happen when I met you. Most of the questions were straightforward, but then I came across one that asked if I had experienced trauma as a child. My heart sank!
My mind started to spin. What was I to write? If I said yes, then I thought you might ask me what had happened. I had never met you, or even seen you from a distance. How could I know that you were the sort of person I would want to discuss that trauma with? How could I know whether you would understand? How could I know why my childhood trauma was relevant, why were you asking?

I felt I was about to be pre-judged because I had experienced childhood trauma, that I had no control over and was not my fault. I wondered if you were going to tell me that the intense pain I was experiencing was ‘all in my head’? I knew it wasn’t, but I instantly felt guarded. Why did you make me feel this way? Why did you increase my anxiety before I had even entered the clinic door? Why did you damage our therapeutic relationship before it had even started?
Was asking me if I had experienced childhood trauma before I had even walked through your door that important? Wouldn’t it have been better if you had got to know me first, judged whether the question was relevant for my individual case or not, and then asked me in a less blunt way, and within the context of a good therapeutic relationship? Do you not have any understanding what effect being asked such a question on a questionnaire might have on me as an individual? It may not bother others, but it really bothers me!
I found it difficult to lie and say ‘no’ and so I left the question blank. I was already nervous about entering your clinic but being faced with that one question made me feel worse, so much so that I can remember those feelings many years later! Do you have any understanding what it is like to have experienced trauma and then find that you are expected to disclose it to a clinician you have never met before? Do you have any idea what it is like to be asked about trauma you have experienced with no explanation about how it might be relevant to your condition? Do you have any idea what might have been going through my mind?
My experience of childhood trauma had little, if any, relevance to our consultation that day. My neuropathic pain was being caused by a prolapsed disc, not by my childhood trauma. Do you really think it was right to give the same questionnaire to all your patients, or to use this type of questionnaire at all? Do the benefits of blanket questionnaires with such questions really outweigh the risks?

I came into your clinic, desperate for help. I felt you were dismissive of me. I was sent a further appointment with you, but I was unhappy with the way you had treated me as a person and so managed to get the appointment changed to another clinician. Do you really think you had the interpersonal skills to open my Pandora’s box of childhood trauma? Don’t you realise that without those skills you could have caused me great harm?
Several years later I met you again. I had been told that I could not have a spinal cord stimulator unless you agreed that I was psychologically ‘fit’. I instinctively knew that I was going to be quizzed about whether I had experienced childhood trauma. I worried I would be pre-judged by you. I worried that the focus of my clinical care would switch to my experience of childhood trauma instead of where it was and needed to be. Thankfully, my concerns were unfounded.
This time you didn’t ask me to fill in a questionnaire before meeting you, and this time we had a sensitive two-way discussion. You didn’t ask me to disclose what my childhood trauma was, and I didn’t have to open my Pandora’s box. This time you concentrated on asking me whether there was a need for me to ‘process’ any trauma further, and you took my word for it when I said there was not.
Your interpersonal skills were much better this time, and I left not feeling judged or stigmatised. I left with the focus of my healthcare the same as it was before. You said you recognised that for me the long-term benefits of experiencing childhood trauma probably outweighed the negatives, and you passed me as psychologically ‘fit’ for a spinal cord stimulator. I left feeling you had given me person-centred, evidence based, healthcare. I left feeling very relieved.
This time I felt your care was informed by a genuine understanding of trauma. I felt you understood the varying impact of trauma on people, both positive and negative, and used that understanding to sensitively support.
We next met when I read your research papers and articles. You emphasised a strong causal link between childhood trauma and persistent pain. You sometimes made me feel that childhood trauma is a purely negative experience, and you sometimes made me feel that the persistent pain I experience must be directly linked to my childhood trauma. You sometimes made me feel that if I hadn’t experienced childhood trauma then I wouldn’t be experiencing persistent pain!
You explained through these research papers and articles, that childhood trauma causes changes in the brain and that these changes are directly related to persistent pain. I’m sure that’s true, and I expect I have changes in my brain associated with my early trauma, but that does not mean that my persistent pain is caused by those changes. Persistent pain is much more complex than that!
You didn’t always portray a balanced picture of the connection between childhood trauma and persistent pain. You didn’t always explain that trauma is just one factor, but there are many more. You didn’t always explain that pain is individual and complex, one size does not fit all!

I have often felt the need to stand up and say that there are positives about experiencing trauma, as well as negatives. I gained many positives from my experience of trauma, including greater resilience, determination, motivation and willpower. These positives have helped me deal with a life with persistent pain, not hindered. I can honestly say that without having experienced trauma my life would be poorer.
I hope the messages you have given about a direct link between trauma and persistent pain have been based on research, but I ask you how good is that research really? There are probably millions of people in the world who have experienced early trauma but don’t have persistent pain. YoungMinds estimate that almost half of all adults living in the UK have experienced at least one form of adversity in their childhood or adolescence, but not all those adults will be living with persistent pain, or even go on to. Could there possibly be an element of bias in your research, and your views? And even if that research has been of a high quality, and unbiased, should that research really be applied to me in a ‘one size fits all’ fashion? Am I not an individual?
Do you really think you can tell if my persistent pain is as a direct result of my early trauma? Do you really think you can tell how significant a part my early trauma might play in my condition? How could you possibly do so? I am hugely self-aware, and I can’t tell what part it plays, so how can you?
I completely understand that for some people unprocessed trauma, or even processed trauma, can have a significant impact on their life, their mental health and on their persistent pain and I have no doubt that any changes in their brain caused by early trauma will have an impact too. Pain is complex and undoubtedly involves a wide range of factors, so why wouldn’t it include these factors too? I am sure that for some people with persistent pain it is helpful if their past experiences of trauma are explored and supported, just like it would be helpful if for example their depression, anxiety or their social circumstances are explored and supported. But let’s not make people feel stigmatised or judged, and let’s proceed with due care. Let’s not make people feel that the trauma they experienced was the main reason they are experiencing persistent pain. How could you possibly know! How do you think that makes some people feel! Let’s be careful with our words and our biases.
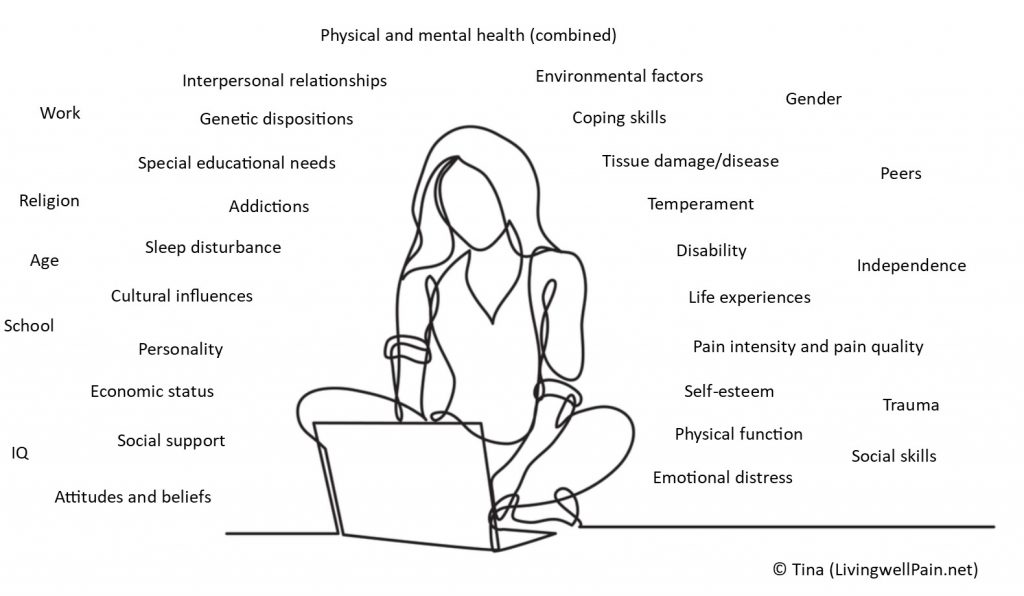
I am lucky, I understand that pain is complex and that there are many causal factors to my pain. I know that who I am, what I feel and what I do has an impact on my persistent pain. I know that part of ‘who I am’ is the trauma I experienced as a young person, but I also know that my experience of trauma was not a wholly negative experience. I know and understand enough that I am prepared to stand strong and say that although childhood trauma may well be one factor in my persistent pain condition, it is by no means the only factor, and nor is it the most dominant or important factor, or the root cause. But why should I feel that I must stand strong? Why have I been made to feel this way?
Why have I been made to feel nervous about telling my clinician I have experienced trauma in case they overly focus on that, and not my whole picture? Why does my heart sink when I see a medical questionnaire? Yes, I probably have changes in my brain related to trauma, and yes there may well be research that indicates a link between childhood trauma and persistent pain, but why have I been made to feel that if I hadn’t experienced that trauma I wouldn’t have persistent pain? Is that fair? Is that right? How do you know?
Important Note
I feel it is important for me to say that these are my personal thoughts only, based on my personal experience of early trauma and my personal persistent pain condition. My thoughts are in no way meant to undermine the superb work that is being done with people who have experienced early trauma and who also experience persistent pain. I am a strong believer in trauma informed care, both in healthcare, social work, education and the criminal justice system. My point is that words matter, biases matter and good therapeutic alliances matter. Most importantly good person-centred, evidence-based, healthcare matters.
This letter is written to a combination of clinicians and clinical researchers/authors that have had an impact on me, either positively or negatively. It is not about any one person. It more likely covers 20 – 30!
I hope it proves helpful to hear this personal view.
My thoughts on what I would like for my future trauma informed persistent pain healthcare have been written HERE.
Tina
@LivingWellPain
www.livingwellpain.net






