‘Pacing’ is a term, and an approach, frequently used by people managing long term health conditions.
It appears to me that there is no agreed understanding as to what ‘pacing’ means when applied to managing a long term condition. I can understand why that might be.
There are hundreds, if not thousands, of different health conditions, and within each named condition different people may be affected in slightly different ways. Many people will experience more than one health condition at a time which just adds to this range and diversity.
It would be impossible to put forward one understanding and approach to ‘pacing’ that would work for every individual and that would work effectively across such a range and complexity of health conditions.
In this blog I hope to briefly explore some different approaches to ‘pacing’, and then look in more detail at how I personally use pacing to self-manage my own persistent pain condition. My pain is largely neuropathic, and I hope to explain why I adopt a slightly different approach to pacing and self-managing my condition, than maybe some other people with persistent pain do.
My approach to ‘pacing’ has been developed to support my individual personality, circumstances and presentation of my health condition, and so cannot be directly applied to others. However, it may be that my thoughts might be helpful to others in developing their own approach to ‘pacing’, in order to help self-manage their own health condition.
In a separate blog I have looked at what happens when pacing ‘goes wrong’ and ‘flares’ occur. That blog is called ‘Persistent Pain ‘Flares” and can be accessed by clicking HERE. It includes suggestions to help recovery from pain flares.
My persistent pain condition
My persistent pain condition started eleven years ago, following a manual handling injury. I currently live with a permanently damaged sciatic nerve root which causes neuropathic pain, some back pain and a shoulder that intermittently causes me difficulties. As well as pain I experience other symptoms such as numbness and unusual leg/foot coldness, and I have an impaired ankle reflex and impaired balance.
Most of my pain and symptoms are neuropathic.
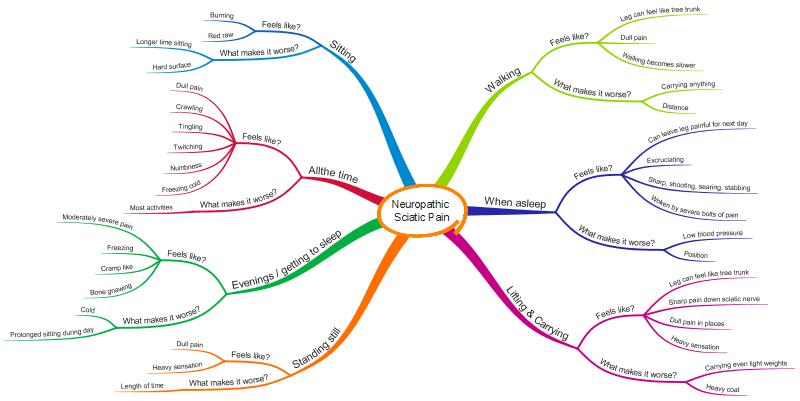
The following is a MindMap which illustrates how I personally experience neuropathic pain. Unfortunately I haven’t worked out a way of showing how often I have any of the symptoms, or how intensely I feel them, but hopefully it will give you an overall picture of how my neuropathic pain condition is experienced by me. Others will experience neuropathic pain differently.
What is ‘pacing’?
I think one of the reasons there isn’t full agreement on the use of the word ‘pacing’ for people self-managing a health condition, and clinicians, is that there isn’t a dictionary definition of pacing which relates particularly well to managing health conditions.
The following are the two ‘best’ dictionary descriptions of pacing I have found to support a healthcare situation, but neither describe how I utilise pacing and in reality they are both quite different to each other.
Dictionary.com provides a suggested definition of ‘pacing’ as ‘to take slow, regular steps’, and the Cambridge English Dictionary suggests ‘to be careful not to do something too quickly, so that you do not get too tired to finish it’.
The following are a few ‘published’ (non-dictionary) descriptions of ‘pacing’ that I think are interesting.
The charity ActionforME supports those living with Chronic Fatigue Syndrome (ME). One of the main symptoms of ME is feeling extremely tired most, or all of the time. There are also other conditions in which fatigue is a dominant feature. ActionforME have produced a booklet which can be found HERE called ‘Pacing for people with M.E’.

In this booklet, ActionforME says ‘Pacing is all about balancing activity and rest to bring about improvements in the way you feel.’ They go on to say ‘To understand pacing it can help to think of your available energy as being like a mobile phone battery. If you completely drain the battery you have to wait to recharge it before you can use the phone again. If you use some of the battery and make regular top ups, then your phone will always be ready to use’.
This seems like a sensible approach to managing a health condition with fatigue as a dominant feature, and also might work for other conditions. However, this approach is not one that I identify with as being helpful in supporting my persistent neuropathic pain condition.
Another description of pacing comes from Pete Moore of The PainToolkit, this time aimed at people living with persistent pain. He says ‘Pacing in short is, taking a break before you need it throughout the day’. Further information about pacing, including a short informative video, can be found HERE.
This is undoubtedly an effective, tried and tested, approach for many people living with persistent pain. I can personally identify in part with this approach, and I do utilise it as part of my own overall ‘pacing’, but for me personally I don’t find this approach on its own sufficiently supports the neuropathic pain elements of my condition. However, it may well work on its own for other people with neuropathic pain, everyone is different.

Oxford University Hospital have published a patient leaflet which says ‘Pacing is a planned approach to increasing your level of activity’. The leaflet can be found HERE. I am sure this is a useful description and approach for many, but it is not sufficient to support my personal persistent pain condition. I am also sure that this is a simplified description for publication purposes, and that the Oxford University Hospital go beyond this in their treatment of patients.
In my view the published approach from Oxford University Hospital is quite different to that of ActionforME, which in turn is quite different to The PainToolkit. I’m sure if I explored the Internet further, or asked a number of different people, I would come up with many other descriptions and approaches to ‘pacing’.
What ‘pacing’ means to me
If I’m honest, ‘pacing’ isn’t a term that I have often used in the management of my own persistent pain condition. However, I think a large part of the way I manage my persistent pain condition could be described as ‘pacing’.
For my own personal persistent pain condition, which is mainly in the context of neuropathic pain, I would view ‘pacing’ as being largely equivalent to my endeavours to avoid known pain triggers and to minimise ‘wind-up’. I will explain ‘wind-up’ shortly.

In addition to minimising ‘wind-up’, I do also incorporate elements of pacing as described by The PainToolkit, largely, but not exclusively, for my non-neuropathic pain elements.
For example, an element of my persistent pain condition relates to back pain. I am able to walk a reasonable distance (for me), but I know a time will come when my back pain will begin to overwhelm me and I will find it difficult to walk much further. In order to avoid that situation then I try to make sure I take a proper break before I reach that ‘overwhelming’ stage. By ‘pacing’ and taking a break I am able to achieve more.
So for me, ‘pacing’ incorporates more than one element. It incorporates minimising ‘wind-up’ and it also incorporates taking breaks, or fundamentally ‘pacing myself’ in order to achieve what I want to with the least pain possible.
Pain ‘Wind-up’
I want to state at the outset of this section that I am not a clinician, and I do not pretend to have a good grasp of understanding the mechanisms of ‘wind up’ when related to pain. One day I would like to write a blog that describes how these mechansims work in detail, but this blog is about how I self-manage the effects of ‘wind-up’ rather than how ‘wind-up’ occurs.
I would also like to state that I fully understand how complex the experience of pain is, some of which I have written about HERE, but it is very difficult for me to write something which I hope will be understandable to others about pacing in the context of my experience of neuropathic pain, which incorporates all the complexities of pain at the same time.

Hopefully though I will be able to provide a very basic and simple description of MY interpretation of ‘wind-up’, describe some of the impact ‘wind-up’ has on me, and describe how I use this simple understanding to help me manage my persistent pain condition.
The way I think of ‘wind-up’ is in two overlapping parts.
Most of my pain is caused by my damaged sciatic nerve root, and is neuropathic in nature. I think of this nerve root as being temperamental in nature, and easily ‘wound-up’. The more it is ‘wound-up’ the more likely I am to experience neuropathic pain from it.
This nerve root is clearly part of my whole body, and my whole body also experiences some ‘wind-up’ of pain. I think of my body as having an overall ‘pain volume dial’ that fundamentally controls how sensitive my overall body is to pain. If I ‘wind-up’ this dial then I am more sensitive to pain, and more likely to experience pain and at a higher intensity.
Clearly if my whole body is in a highly pain sensitive state then I am more likely to experience pain not only from my sciatic nerve root, but from other parts of my body also.
I will try and explain a little more about what I will now call ‘whole body pain wind-up’ and ‘neuropathic pain wind-up’, without going into too much technical detail, below.
Whole body pain ‘wind-up’
When you have experienced pain over a significant period of time, as I have, your body is likely to undergo some changes. The repeated pain you experience can modify the way that your central nervous system works, and you can become overall more sensitive to pain. Your pain sensitivity dial is turned up and you may experience amplified pain.

Unfortunately, like many others, I have lived with pain for so long that I no longer know what is ‘normal’ pain, and I can’t always tell if my pain sensitivity dial is turned up, or not. I am fairly sure I do experience amplified pain, at least at times, but my judgement as to what is ‘normal’ pain and what is amplified is impaired.
The pain sensitivity dial doesn’t get turned up only once in response to the complexities of persistent pain, it is something that is variable, and something that can be positively influenced by good pain self-management, including ‘pacing’.
Neuropathic pain ‘wind-up’
As part of my long-term persistent pain condition, and related to my damaged sciatic nerve root, I experience neuropathic pain ‘wind up’, which I hope through examples to explain below.
Minimising this ‘wind-up’ is fundamentally my equivalent of ‘pacing’ in MY neuropathic pain context.
I have various triggers to my neuropathic pain, and other symptoms (eg numbness) which I have illustrated in the mind map below:

Some of these are physical triggers and some are related to my mental and emotional state (eg work stress). Sometimes these triggers will cause an immediate response of pain, and sometimes they won’t. I cannot reliably predict when I am likely to experience immediate pain, and when I’m not.
For example more often than not if my sciatic nerve is ‘tugged’ then I am likely to experience immediate pain, but not always. For example if I get out of the passenger door of a car on my steep drive then I am quite likely to experience severe pain, but this doesn’t always happen. If I lift anything and carry it, for even a relatively short distance, then I am likely to experience both pain and numbness, but the intensity of both symptoms will vary. If I sit on a hard surface then I am likely to experience immediate pain, but there is no certainty to the level of that pain or its duration.
What I feel happens is that my sciatic nerve root is ‘irritated’ by the various triggers I experience, even if this ‘irritation’ doesn’t result in immediate pain. As the day goes on there is an accumulation of all these ‘irritations’ and my nerve root is effectively ‘wound up’.
The result of this ‘wind-up’ for me is that as I go through the day and into the evening my pain sensitivity becomes increased, and I become more likely to experience pain than say I might have done in the morning with a similar trigger.

For example, if I sit on a hard surface in the evening then I am more likely to experience pain, or worse pain, than if I sat on the same hard surface in the morning, because my sciatic nerve root has effectively been ‘wound-up’ and has become more sensitive to triggers as the day has passed.
I should add that this is how my personal condition affects me, and this may well not be the same for other people, even with a seemingly similarly damaged sciatic nerve root. There is huge variation as to how people are affected by a health condition, and how and when they experience pain.
If I have experienced a lot of pain triggers during the day, for example if I have sat quite still for extensive periods of the day, then I am quite likely to experience severe neuropathic pain later in the evening and maybe at sporadic times during the night. As far as I can tell these episodes of severe pain aren’t in response to any particular trigger occurring at that time, but seem to somehow be in response to the number and type of pain triggers I experienced that day.
I visualise this in a similar way to a mother being ‘wound up’ by their child. The more and more the child ‘pokes’ and ‘aggravates’ their mother through the day the more temperamental and explosive she may become. I view my sciatic nerve root as being temperamental, particularly later in the day and evening, and at times explosive!
Fortunately I find that this accumulated irritation and wind-up of my sciatic nerve root usually dissipates over night and I start the next day with ‘a clean slate’. It is as though my nerve root and pain condition are ‘reset’ during the night.

However, there are times when this ‘reset’ doesn’t fully happen, and I start the following day with my sciatic nerve already in an irritated and wound-up state. This makes it likely that I will experience increased pain and symptoms as I go through that day and into the night.
If this incremental increase of irritation and wind up goes on for a number of days then I am likely to go into a ‘flare up’ situation.
In order to reduce the likelihood of a significant ‘flare up’ of my condition, and in order to minimise the pain and other symptoms I experience on a daily basis, I actively seek to minimise the wind-up of my nerve root.

It is this positive avoidance and management of pain triggers that forms the basis of my pain self-management, and my ‘pacing’. I have written more about how I self-manage my predominantly neuropathic pain HERE and HERE.
Pacing in the context of MY neuropathic pain

Living with persistent pain, particularly I think neuropathic pain, can be difficult. However I have found that by seeking to understand my condition, including what makes it worse or better, and by adopting pro-active self-management techniques, including ‘pacing’, I have been able to live well with pain.
I hope the description I have given of my approach to ‘pacing’ might help others living with persistent pain, particularly if they have neuropathic pain, to develop their own approach.
There is no ‘one-size fits all’. Each of us needs to work out our own way of managing our persistent pain or other long term condition. This is merely mine. I hope it may be helpful for others to read.
As ever I am very interested to hear any thoughts and comments on this post.
I would like to acknowledge the help and support my physiotherapist @MattLowPT has given me. He has patiently, and compassionately, helped me to understand my persistent pain condition and has helped me to develop my pain management techniques.




Amazing!!! I’m a MSK physio of a dozen years experience, and this blog succinctly describes much of what I try (blunderingly) to explain to patients with chronic pain. The advice is practical, easy to understand, and reflects the complex (and sometimes baffling) behaviour of pain and its foibles.
Wow! Thank you.
I agree – pain has a lot of foibles!
Amazing, this is actually describing myself. I received this information from an MSK Physio, as I am currently going through a “flare up” . So much of this makes sense and is helping me to understand, re adjust and go forward.
Thank you.